Introduction
Do not let yourself be misled by the fear campaign, pointing to a Worldwide coronavirus calamity with repeated “predictions” that hundreds of thousands of people are going to die.
These are boldface lies. Scientific assessments of the health impacts of the COVID-19 have been withheld, they do not make the headlines.
Examine the contradictory headlines:
Screenshot The Hill
According to the WHO and John Hopkins Medicine (see below), the risks of dying from influenza are higher than from COVID-19.
Moreover, the media fails to acknowledge that there are simple and effective treatments for COVID-19. In fact, the reports on the treatment of COVID-19 are being suppressed. And the issue of “recovery” is barely mentioned.
Persistent headlines and TV reports. Fear and panic. Neither the WHO nor our governments have taken the trouble to reassure us.
According to latest media hype, citing and often distorting scientific opinion (CNBC)
Statistical Models by Washington think tanks predict a scenario of devastation suggesting that “more than a million Americans could die if the nation does not take swift action to stop its spread as quickly as possible”.
One model from the Centers for Disease Control and Prevention (CDC) suggested that between
160 million and 210 million Americans could contract the disease over as long as a year. Based on mortality data and current hospital capacity, the number of deaths under the CDC’s scenarios ranged from 200,000 to as many as 1.7 million. (
The Hill, March 13, 2020)
The Unspoken Truth: Unprecedented Global Crisis
The unspoken truth is that the novel coronavirus provides a pretext to powerful financial interests and corrupt politicians to trigger the entire World into a spiral of mass unemployment, bankruptcy, extreme poverty and despair.
This is the true picture of what is happening. “Planet Lockdown” is an encroachment on civil liberties. Entire national economies are in jeopardy. In some countries martial law has been declared.
This crisis is unprecedented in World history. It is destabilizing and destroying people’s lives Worldwide. It’s a “War against Humanity”.
While it is presented to World public opinion as a WHO global health emergency, what is really at stake are the mechanisms of “economic warfare” sustained by fear and intimidation, with devastating consequences.
The economic and social impacts far exceed those attributed to the coronavirus. Cited below are selected examples of a global process:
- Massive job losses and layoffs in the US, with more than 10 million workers filing claims for unemployment benefits.
- In India, a 21 days lockdown has triggered a wave of famine and despair affecting millions of homeless migrant workers all over the country. No lockdown for the homeless: “too poor to afford a meal”.
- The impoverishment in Latin America and sub-Saharan Africa is beyond description. For large sectors of the urban population, household income has literally been wiped out.
- In Italy, the destabilization of the tourist industry has resulted in bankruptcies and rising unemployment.
- In many countries, citizens are the object of police violence. Five people involved in protests against the lockdown were killed by police in Kenya and South Africa.
The WHO’s global health emergency was declared on January 30th, when there were 150 confirmed cases outside China. From the outset it was based on a big lie.
Moreover, the timing of the WHO emergency coincided with America’s ongoing wars as well simmering financial instability on the World’s stock markets.
To reverse the tide, we must confront the lies. And the lies are overwhelming. A counter propaganda initiative is required.
When the Lie becomes the Truth, there is No Moving Backwards.
***
Part II
The Second Part of this article will largely focus on the following issues:
- the definition of COVID-19 and the assessment of the number of “confirmed cases”,
- the risks to people’s health,
- how the alleged epidemic is measured and identified.
The Spread of the COVID-19 Infection
In many countries including the US, there is no precise lab test which will identify COVID-19 as the cause of a positive infection. Meanwhile the media will not only quote unreliable statistics, it will forecast a doomsday scenario.
Let us put the discussion on COVID-19 in context.
What is a Human Coronavirus. “Coronaviruses are everywhere”. They are categorized as “the second leading cause of the common cold (after rhinoviruses)”. Since the 2003 outbreak of SARS (severe acute respiratory syndrome coronavirus), several (new) corona viruses were identified. COVID-19 is categorized as a novel or new corona virus initially named SARS-CoV-2.
According to Dr. Wolfgang Wobag, pneumonia is “regularly caused or accompanied by corona viruses”. And that has been the case for many years prior to the identification of the COVID-19 in January 2020:
[It is a] well-known fact that in every “flu wave” 7-15% of acute respiratory illnesses (ARI) are coming along with coronaviruses”
The COVID-19 belongs to the family of coronviruses which trigger colds and seasonal influenza. We will also address the lab tests required to estimate the data as well as the spread of the COVID-19. The WHO defines the COVID-19 as follows:
“The most commonly reported symptoms [of COVID-19] included fever, dry cough, and shortness of breath, and most patients (80%) experienced mild illness. Approximately 14% experienced severe disease and 5% were critically ill. Early reports suggest that illness severity is associated with age (>60 years old) and co-morbid disease.” (largely basing on WHO’s assessment of COVID-19 in China)
The overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.“
These assessments confirm that COVID-19 is akin to seasonal influenza and pneumonia, categorized as contagious respiratory infections.
If the above definitions had made the headlines, there would have been no fear and panic.
The COVID-19. Tests and Data Collection
The H1N1 Pandemic 2009. Déjà Vu
This is not the first time that a global health emergency has been called by the WHO in close liaison with Big Pharma.
In 2009, the WHO launched the H1N1 Swine Flu Pandemic predicting that “as many as 2 billion people could become infected over the next two years — nearly one-third of the world population.” (World Health Organization as reported by the Western media, July 2009).
While creating an atmosphere of fear and insecurity, pointing to am impending global public health crisis, the WHO acknowledged that the underlying symptoms were moderate and that “most people will recover from swine flu within a week, just as they would from seasonal forms of influenza” (WHO statement, quoted in the Independent, August 22, 2009).
And President Obama’s Council of Advisors on Science and Technology stated with authority and determination that “the H1N1 pandemic ‘a serious health threat; to the U.S. — not as serious as the 1918 Spanish flu pandemic but worse than the swine flu outbreak of 1976.”
Spinning Fear and Panic Across America. Analysis of COVID-19 Data
H1N1 Fake Date
In many regards, the H1N1 2009 pandemic reveals the problems of data collection and analysis in relation to COVID-19
Following the outbreak of the H1N1 swine flu in Mexico, the data collection was at the outset scanty and incomplete, as confirmed by official statements. The Atlanta based Center for Disease Control (CDC) acknowledged that what was being collected in the US were figures of “confirmed and probable cases”. There was, however, no breakdown between “confirmed” and “probable”. In fact, only a small percentage of the reported cases were “confirmed” by a laboratory test.
There was no attempt to improve the process of data collection in terms of lab confirmation. In fact quite the opposite. Following the level 6 Pandemic announcement, both the WHO and the CDC decided that data collection of individual confirmed and probable cases was no longer necessary to ascertain the spread of swine flu
. One month after the announcement of the level six pandemic, the WHO discontinued the collection of “confirmed cases”. It did not require member countries to send in figures pertaining to confirmed or probable cases.
WHO, Briefing note, 2009)
Based on incomplete, scanty and suppressed data, the WHO nonetheless predicted with authority that: “as many as 2 billion people could become infected over the next two years — nearly one-third of the world population.” (World Health Organization as reported by the Western media, July 2009).
In 2010, Dr. Margaret Chan and the WHO were the object of an investigation by the European Parliament:
“Confirmed Cases”: The CDC Methodology
The CDC methodology in 2020 is broadly similar (with minor changes in terminology) to that applied to the H1N1 pandemic in 2009.
Presumptive vs. Confirmed Cases
According to the CDC the data presented for the United States “include both “confirmed” and “presumptive” positive cases of COVID-19 reported to CDC or tested at CDC since January 21, 2020″.
The presumptive positive data does not confirm coronavirus infection: Presumptive testing involves “chemical analysis of a
sample that
establishes the possibility that a substance [COVID-19] is present“ (emphasis added). But it does not confirm the COVID-19. The presumptive test must then be sent for confirmation to an accredited government health lab. (For further details see: Michel Chossudovsky,
Spinning Fear and Panic Across America. Analysis of COVID-19 Data, March 20, 2020)
How is the COVID-19 Data Tabulated?
The presumptive (PC) and confirmed cases (CC) are lumped together. And the total number (PC + CC ) constitutes the basis for establishing the data for COVID-19 infection. It’s like adding apples and oranges. The total figure (PC+CC) categorized as “Total cases” is meaningless. It does not measure positive COVID-19 Infection.
CDC Data for April 5, 2020
But there is another important consideration: the required CDC lab test pertaining to CC (confirmed cases) is intended to “confirm the infection”. But does it confirm that the infection was caused by COVID-19?
The COVID-19 is a coronvirus which is associated with the broad symptoms of seasonal influenza and pneumonia. Are the lab exams pertaining to COVID-19 (confirmed cases) in a position to establish unequivocally the prevalence of COVID-19 positive infection?
Results are for the identification of 2019-nCoV RNA. The 2019-nCoV RNA is generally detectable in upper and lower respiratory specimens during infection. Positive results are indicative of active infection with 2019-nCoV but do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease. Laboratories within the United States and its territories are required to report all positive results to the appropriate public health authorities.
Negative results do not preclude 2019-nCoV infection and should not be used as the sole basis for treatment or other patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information.
What this suggests is that a positive infection could be the result of other viruses as well as other corona viruses. (i.e. related to seasonal influenza or pneumonia).
Moreover, the second paragraph suggests that “Negative Results” of the lab test does not preclude a positive COVID-12 infection. But neither do the “combined clinical observations, etc … “.
These criteria and CDC guidelines are contradictory and inevitably subject to error. Since January, these “positive test results” of the RT-PCR Diagnostic Panel do not prove that COVID-19 is the cause of a positive infection for the COVID-19. (also referred to as 2019-nCoV and SARS-CoV-2). (See annex below).
Where does the bias come in?
Various coronaviruses are there in the tested specimen. Does the test identify COVID-19?
Has the COVID-19 been singled out as the source of an active infection, when the infection could be the result of other viruses and/or bacteria?
Important Question?
Are the tests conducted in the US since January 2020 (pertaining to upper and lower respiratory specimens) which confirm infection from one or more causes (without proof of COVID-19) entered in the CDC data banks as “confirmed cases” of COVID-19?
As outlined by the CDC: “The agent detected may not be the definite cause of disease.”
Moreover, the presumptive cases” referred to earlier –which do not involve the test of a respiratory specimen– are casually lumped together with “confirmed cases” which are then categorized as “Total Cases”.
Another fundamental question: What is being tested?
Inasmuch as COVID-19 and Influenza have similar symptoms, to what extent are the data pertaining to COVID-19 “overlapping” with those pertaining to viral seasonal influenza and pneumonia?
The test pertaining to active infection could be attributed either to influenza or COVID-19, or both?
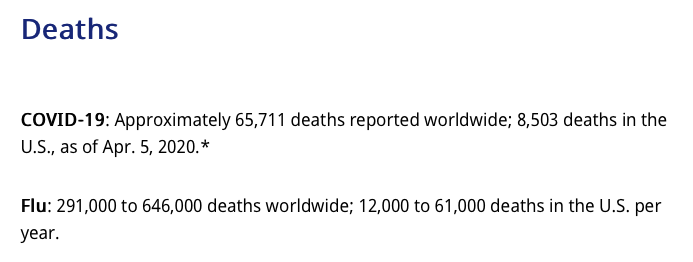
What is More Dangerous: Seasonal Influenza or COVID-19?
Seasonal Influenza –which has never been the object of a lockdown– appears from the recorded data on mortality to be “more dangerous” than COVID-19?
Based on the figures below, the recorded annual death rate pertaining to Influenza is substantially higher than that pertaining to COVID-19. (This is a rough comparison, given the fact that the recorded data pertaining to COVID-19 is not on an annual basis).
(Globally, all countries and territories): 40,598 deaths (recorded up until April 1, 2020).
The estimates of annual mortality pertaining to Influenza:
Historically of the order of 250 000 to 500 000 annually (globally). (WHO).
The most recent WHO estimates (2017):
290 000 – 650 000 deaths globally (annual).
ANNEX
Note: Two important texts
Intended Use
The CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel is a real-time RT-PCR test intended for the qualitative detection of nucleic acid from the 2019-nCoV in upper and lower respiratory specimens (such as nasopharyngeal or oropharyngeal swabs, sputum, lower respiratory tract aspirates, bronchoalveolar lavage, and nasopharyngeal wash/aspirate or nasal aspirate) collected from individuals who meet 2019-nCoV clinical and/or epidemiological criteria (for example, clinical signs and symptoms associated with 2019-nCoV infection, contact with a probable or confirmed 2019-nCoV case, history of travel to geographic locations where 2019-nCoV cases were detected, or other epidemiologic links for which 2019-nCoV testing may be indicated as part of a public health investigation). Testing in the United States is limited to laboratories certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. § 263a, to perform high complexity tests.
Results are for the identification of 2019-nCoV RNA. The 2019-nCoV RNA is generally detectable in upper and lower respiratory specimens during infection. Positive results are indicative of active infection with 2019-nCoV but do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease. Laboratories within the United States and its territories are required to report all positive results to the appropriate public health authorities.
Negative results do not preclude 2019-nCoV infection and should not be used as the sole basis for treatment or other patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information.
Testing with the CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel is intended for use by trained laboratory personnel who are proficient in performing real-time RT-PCR assays. The CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel is only for use under a Food and Drug Administration’s Emergency Use Authorization.
Summary and Explanation
An outbreak of pneumonia of unknown etiology in Wuhan City, Hubei Province, China was initially reported to WHO on December 31, 2019. Chinese authorities identified a novel coronavirus (2019-nCoV), which has resulted in thousands of confirmed human infections in multiple provinces throughout China and many countries including the United States. Cases of asymptomatic infection, mild illness, severe illness, and some deaths have been reported.
The CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel is a molecular in vitro diagnostic test that aids in the detection and diagnosis 2019-nCoV and is based on widely used nucleic acid amplification technology. The product contains oligonucleotide primers and dual-labeled hydrolysis probes (TaqMan®) and control material used in rRT-PCR for the in vitro qualitative detection of 2019-nCoV RNA in respiratory specimens.
The term “qualified laboratories” refers to laboratories in which all users, analysts, and any person reporting results from use of this device should be trained to perform and interpret the results from this procedure by a competent instructor prior to use.
Principles of the Procedure
The oligonucleotide primers and probes for detection of 2019-nCoV were selected from regions of the virus nucleocapsid (N) gene. The panel is designed for specific detection of the 2019-nCoV (two primer/probe sets). An additional primer/probe set to detect the human RNase P gene (RP) in control samples and clinical specimens is also included in the panel.
RNA isolated and purified from upper and lower respiratory specimens is reverse transcribed to cDNA and subsequently amplified in the Applied Biosystems 7500 Fast Dx Real-Time PCR Instrument with SDS version 1.4 software. In the process, the probe anneals to a specific target sequence located between the forward and reverse primers. During the extension phase of the PCR cycle, the 5’ nuclease activity of Taq polymerase degrades the probe, causing the reporter dye to separate from the quencher dye, generating a fluorescent signal. With each cycle, additional reporter dye molecules are cleaved from their respective probes, increasing the fluorescence intensity. Fluorescence intensity is monitored at each PCR cycle by Applied Biosystems 7500 Fast Dx Real-Time PCR System with SDS version 1.4 software.
Detection of viral RNA not only aids in the diagnosis of illness but also provides epidemiological and surveillance information.
The CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel is a real-time RT-PCR test intended for the qualitative detection of nucleic acid from the 2019-nCoV in upper and lower respiratory specimens (such as nasopharyngeal or oropharyngeal swabs, sputum, lower respiratory tract aspirates, bronchoalveolar lavage, and nasopharyngeal wash/aspirate or nasal aspirate) collected from individuals who meet 2019-nCoV clinical and/or epidemiological criteria (for example, clinical signs and symptoms associated with 2019-nCoV infection, contact with a probable or confirmed 2019-nCoV case, history of travel to geographic locations where 2019-nCoV cases were detected, or other epidemiologic links for which 2019-nCoV testing may be indicated as part of a public health investigation). Testing in the United States is limited to laboratories certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. § 263a, to perform high complexity tests.
Results are for the identification of 2019-nCoV RNA. The 2019-nCoV RNA is generally detectable in upper and lower respiratory specimens during infection. Positive results are indicative of active infection with 2019-nCoV but do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease. Laboratories within the United States and its territories are required to report all positive results to the appropriate public health authorities.
Negative results do not preclude 2019-nCoV infection and should not be used as the sole basis for treatment or other patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information.
Testing with the CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel is intended for use by trained laboratory personnel who are proficient in performing real-time RT-PCR assays. The CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel is only for use under a Food and Drug Administration’s Emergency Use Authorization.
CDC is working to develop a new laboratory test to assist with efforts to determine how much of the U.S. population has been exposed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.
The serology test will look for the presence of antibodies, which are specific proteins made in response to infections. Antibodies can be found in the blood and in other tissues of those who are tested after infection. The antibodies detected by this test indicate that a person had an immune response to SARS-CoV-2, whether symptoms developed from infection or the infection was asymptomatic. Antibody test results are important in detecting infections with few or no symptoms.
Initial work to develop a serology test for SARS-CoV-2 is underway at CDC. In order to develop the test, CDC needs blood samples from people who had COVID-19 at least 21 days after their symptoms first started. Researchers are currently working to develop the basic parameters for the test, which will be refined as more samples become available. Once the test is developed, CDC will need additional samples to evaluate whether the test works as intended.The original source of this article is Global ResearchCopyright ©
Prof Michel Chossudovsky, Global Research, 2020
River to Sea Uprooted Palestinian
Uprooted Palestinian 
 Uprooted Palestinian
Uprooted Palestinian 















No comments:
Post a Comment